Managing Recurrent Incisional Hernia with Severe Small Bowel Adhesion and Subacute Obstruction
Add to
Share
1,668 views
Report
2 years ago
Description
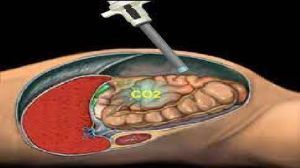
Introduction: Recurrent incisional hernias accompanied by severe small bowel adhesions and subacute obstructions pose a significant challenge in surgical management. This essay delves into the complexities involved in addressing these interconnected conditions, exploring the diagnostic and treatment approaches necessary to provide effective care for patients facing this complex surgical challenge. Understanding Recurrent Incisional Hernia: A recurrent incisional hernia refers to the protrusion of abdominal organs or tissues through a previous surgical incision that has failed to heal properly. It can occur due to factors such as wound dehiscence, weak tissue integrity, or inadequate closure techniques. These hernias often demand surgical intervention to alleviate symptoms and prevent further complications. The Impact of Severe Small Bowel Adhesion: Small bowel adhesions are fibrous bands that form between loops of the small intestine and surrounding tissues, resulting from previous surgeries, infections, or inflammation. Severe small bowel adhesions can lead to bowel obstructions, which impede the normal passage of intestinal contents and cause symptoms such as abdominal pain, bloating, and nausea. Managing Subacute Obstruction: Subacute obstruction refers to a partial blockage of the bowel, which can be caused by adhesions, hernias, or other factors. The condition manifests with intermittent symptoms, including abdominal pain, distention, and changes in bowel movements. Prompt intervention is crucial to prevent the progression to complete bowel obstruction, which may require emergency surgery. The Surgical Challenge: Addressing recurrent incisional hernias with severe small bowel adhesion and subacute obstruction requires a comprehensive and multidisciplinary approach. Key aspects of managing this complex challenge include: Thorough diagnostic evaluation: Accurate diagnosis is vital to understand the extent and nature of the hernia recurrence, small bowel adhesions, and the severity of the obstruction. Imaging studies, such as computed tomography (CT) scans, can aid in assessing the anatomical details and guide surgical planning. Individualized treatment plan: Each case demands a tailored treatment plan based on the patient's overall health, the extent of the hernia and adhesions, and the severity of the obstruction. Surgery is often the primary intervention, and various techniques may be employed, such as hernia repair, adhesiolysis, and bowel resection if necessary. Minimally invasive approaches: Whenever feasible, laparoscopic or robotic-assisted techniques can be utilized to minimize surgical trauma, reduce postoperative pain, and facilitate faster recovery. These advanced techniques offer a less invasive option compared to traditional open surgeries, particularly beneficial for patients with complex conditions. Multidisciplinary collaboration: Given the complexity of recurrent incisional hernias with severe small bowel adhesion and subacute obstruction, collaboration between surgeons, gastroenterologists, radiologists, and other specialists is crucial. Their combined expertise ensures comprehensive evaluation, optimal treatment planning, and postoperative care to achieve the best possible outcomes for patients. Recurrent incisional hernia with severe small bowel adhesion and subacute obstruction poses a complex surgical challenge that requires careful diagnosis and treatment. This description explores the intricacies involved in managing these interrelated conditions, highlighting the importance of personalized care and multidisciplinary collaboration to achieve successful outcomes. Recurrent incisional hernia refers to the protrusion of abdominal organs or tissues through a previous surgical incision, often requiring surgical intervention. Severe small bowel adhesion involves the formation of fibrous bands between the small intestine and surrounding tissues, leading to potential bowel obstructions. Subacute obstruction is a partial blockage of the bowel that presents intermittent symptoms. Managing this complex scenario involves comprehensive diagnostic evaluation to assess the extent of hernia recurrence, severity of adhesions, and obstruction. Tailored treatment plans are then devised, considering factors such as the patient's overall health and the specific conditions involved. Surgical interventions, including hernia repair, adhesiolysis, and bowel resection if necessary, are commonly employed. Minimally invasive approaches, such as laparoscopic or robotic-assisted techniques, are preferred when feasible, as they minimize surgical trauma and promote faster recovery. Multidisciplinary collaboration among surgeons, gastroenterologists, radiologists, and other specialists is essential for comprehensive evaluation, treatment planning, and postoperative care. In summary, managing recurrent incisional hernia with severe small bowel adhesion and subacute obstruction requires individualized approaches, advanced surgical techniques, and collaborative efforts. By combining expertise from different specialties, healthcare professionals can navigate the complexities of this condition and provide optimal care for patients. Conclusion: Managing recurrent incisional hernia with severe small bowel adhesion and subacute obstruction presents a complex challenge in surgical practice. By employing a multidisciplinary approach, personalized treatment plans, and leveraging minimally invasive techniques, surgeons can navigate this complexity and provide effective management for patients. Understanding the interconnected nature of these conditions and tailoring interventions based on individual patient needs are essential to achieve successful outcomes in this complex surgical scenario.
Similar Videos