Transvaginal Ovary Extraction via Laparoscopic Salpingo-Oophorectomy
Add to
Share
1,259 views
Report
1 year ago
Description
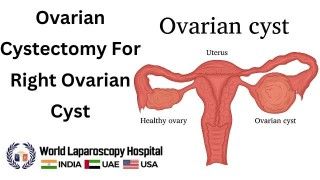
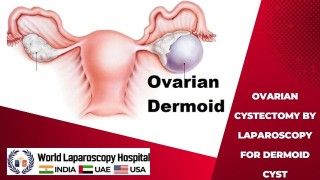
Introduction: Transvaginal ovary extraction, performed using the laparoscopic salpingo-oophorectomy technique, represents a cutting-edge advancement in gynecological surgery. This minimally invasive procedure offers numerous benefits for patients, including reduced postoperative pain, quicker recovery times, and enhanced cosmetic outcomes. By exploring the key aspects of this innovative technique, its indications, advantages, and potential complications, we can better understand how it contributes to optimal patient care. 1. The Laparoscopic Salpingo-Oophorectomy Procedure: Laparoscopic salpingo-oophorectomy is a surgical procedure that involves the removal of one or both ovaries and fallopian tubes through small incisions in the abdomen. During the transvaginal approach, the surgeon accesses the pelvic region through the vaginal canal, eliminating the need for additional external incisions on the abdomen. 2. Indications for Transvaginal Ovary Extraction: This technique is typically indicated for various gynecological conditions, including but not limited to: a. Benign Ovarian Cysts: Transvaginal ovary extraction is an effective option for the removal of non-cancerous cysts that can cause pain, discomfort, or hormonal imbalances. b. Endometriosis: For patients with endometriosis affecting the ovaries or fallopian tubes, laparoscopic salpingo-oophorectomy can provide symptomatic relief and improve fertility prospects. c. Ovarian Tumors: In cases of suspected or confirmed ovarian tumors, this approach allows for precise removal of affected tissues while preserving the uterus and other reproductive organs. d. Risk Reduction: High-risk patients with a family history of ovarian cancer or carrying genetic mutations like BRCA1/2 may opt for prophylactic ovary removal to reduce the risk of developing ovarian cancer. 3. Advantages of Transvaginal Ovary Extraction: a. Minimally Invasive: The transvaginal approach significantly reduces trauma to the abdominal wall, resulting in less postoperative pain, reduced risk of infection, and a shorter hospital stay. b. Improved Cosmetic Outcomes: The absence of external abdominal incisions minimizes visible scarring, contributing to enhanced patient satisfaction. c. Faster Recovery: Patients undergoing laparoscopic salpingo-oophorectomy generally experience quicker recovery times, allowing them to resume their daily activities sooner. d. Reduced Blood Loss: The precise nature of the laparoscopic procedure helps minimize blood loss during surgery, enhancing overall patient safety. 4. Potential Complications and Considerations: Although transvaginal ovary extraction is considered a safe and effective procedure, certain complications may arise, including: a. Vaginal Injury: Careful surgical planning and expertise are essential to avoid inadvertent injury to the vaginal wall during the transvaginal approach. b. Bleeding: As with any surgery, there is a risk of intraoperative or postoperative bleeding that may necessitate further intervention. c. Infection: Vigilant postoperative care and antibiotic prophylaxis help minimize the risk of infection at the surgical site. d. Conversion to Laparotomy: In some cases, technical challenges or unexpected findings may require converting to traditional open surgery (laparotomy). Gynecological surgeries have undergone revolutionary changes over the years, transitioning from traditional open procedures to minimally invasive techniques. Among these advancements, transvaginal ovary extraction through laparoscopic salpingo-oophorectomy stands out as a groundbreaking procedure that exemplifies the pursuit of optimal patient care. By providing a comprehensive and in-depth exploration of this innovative approach, its historical context, procedural intricacies, patient benefits, and future implications, we can gain profound insights into how it is reshaping the landscape of gynecological surgery. Historical Context and Evolution: The evolution of gynecological surgery is closely intertwined with a relentless quest for less invasive methods to minimize patient discomfort and promote quicker recovery. Traditional open surgeries, while effective, often came with significant postoperative pain, prolonged hospital stays, and conspicuous scarring. In the late 20th century, laparoscopy emerged as a game-changer, enabling surgeons to perform various gynecological procedures through small incisions. The advent of laparoscopic salpingo-oophorectomy in the early 21st century revolutionized the field once again, taking minimally invasive gynecological surgery to new heights. Initially introduced for the removal of ovarian cysts and benign tumors, this technique has expanded its applications to encompass a wide range of gynecological conditions, elevating the standard of patient care. The Transvaginal Approach and Surgical Technique: The hallmark of transvaginal ovary extraction is its unique approach that utilizes the vaginal canal as the primary access point to the pelvic region. Unlike traditional laparoscopic procedures that require several small incisions on the abdomen, this technique minimizes external scarring and offers a more discreet and cosmetically appealing outcome. The procedure typically involves the following steps: a. Patient Preparation: Adequate patient evaluation and preparation are essential to ensure eligibility for the transvaginal approach. Factors like pelvic anatomy, previous surgeries, and medical history are carefully assessed to determine the feasibility of the procedure. b. Anesthesia and Instrument Placement: The patient is placed under general anesthesia, and trocars (small, hollow tubes) are inserted into the abdominal cavity through the vaginal canal. Carbon dioxide gas is introduced to create space for the surgeon to maneuver the laparoscopic instruments. c. Visualization and Ovary Extraction: A laparoscope, a thin, lighted tube with a camera, provides real-time visuals of the pelvic organs on a monitor. The surgeon skillfully manipulates the instruments to isolate the affected ovary or ovaries and carefully removes them, often alongside the fallopian tubes. d. Closure and Recovery: After ovary extraction, the instruments are removed, and the vaginal canal is closed using dissolvable sutures. The patient is then carefully monitored during the recovery period. Advantages for Optimal Patient Care: Transvaginal ovary extraction via laparoscopic salpingo-oophorectomy offers numerous advantages that significantly contribute to optimal patient care: a. Minimized Pain and Discomfort: Compared to open surgeries, the transvaginal approach results in reduced postoperative pain and discomfort, enabling patients to recover more comfortably. b. Accelerated Recovery: Shorter hospital stays and quicker recovery times allow patients to return to their daily activities and routines sooner, promoting overall well-being and satisfaction. c. Enhanced Cosmesis: The absence of external abdominal incisions diminishes visible scarring, providing patients with improved cosmetic outcomes and heightened self-confidence. d. Preservation of Reproductive Organs: This technique allows the surgeon to precisely remove the affected ovaries while preserving the uterus and other reproductive organs, offering women greater fertility prospects and overall reproductive health. Future Implications and Ongoing Advancements: Transvaginal ovary extraction represents a paradigm shift in gynecological surgery, and its continued development is expected to have far-reaching implications. As surgeons refine their techniques and technology advances further, the scope of applications for this approach is likely to expand. Continued research and innovation may lead to even more tailored and patient-centric approaches to gynecological surgeries, ultimately raising the bar for optimal patient care. Conclusion: Transvaginal ovary extraction via laparoscopic salpingo-oophorectomy represents a remarkable advancement in gynecological surgery. Its minimally invasive nature, coupled with reduced postoperative pain and faster recovery times, fosters optimal patient care and satisfaction. As with any medical procedure, careful patient selection, surgical expertise, and diligent postoperative care are vital to ensure successful outcomes and minimize potential complications. The continued refinement of this technique promises further improvements in gynecological care, benefitting countless women worldwide.
Similar Videos