Major Vessel Bleeding and the Risk of Air Embolism
Add to
Share
1,245 views
Report
10 months ago
Description
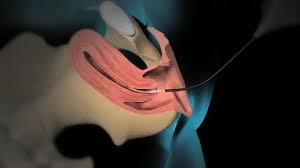
Major Vessel Bleeding and Air Embolism Risks in Surgical Procedures is a critical topic that delves into the significant dangers posed by these complications during various surgical interventions. Major vessel bleeding, often resulting from trauma, surgical injury, or underlying medical conditions, can lead to rapid blood loss, hypovolemic shock, and potentially fatal outcomes if not promptly managed. On the other hand, air embolism occurs when air enters the vascular system, with venous air embolism being more common due to lower venous pressures. Both complications can result in severe physiological disruptions, necessitating swift and effective intervention. This topic explores the pathophysiology of major vessel bleeding and air embolism, identifying key risk factors associated with cardiovascular, thoracic, and neurosurgical procedures. It also covers the clinical manifestations of these conditions, emphasizing the importance of early detection and diagnosis through advanced imaging techniques and intraoperative monitoring. Effective management strategies are crucial for mitigating the impact of these complications. This includes immediate control measures for bleeding, volume resuscitation, and surgical repair techniques, alongside preventive measures and emergency management protocols for air embolism, such as positioning, aspiration, and hyperbaric oxygen therapy. Understanding the complexities of major vessel bleeding and air embolism, and the latest advancements in surgical technology and techniques, is essential for improving patient outcomes and reducing the incidence of these life-threatening events in surgical practice. Major Vessel Bleeding and Air Embolism Risks in Surgical Procedures examines the critical complications that can arise during surgical interventions, posing significant threats to patient safety and outcomes. This topic is particularly pertinent in the context of cardiovascular, thoracic, and neurosurgical operations, where the proximity to major blood vessels and the potential for air introduction into the vascular system are high. Major Vessel Bleeding: Major vessel bleeding involves significant hemorrhage from large arteries or veins, such as the aorta, carotid arteries, or femoral arteries. Causes can include traumatic injuries, surgical errors, ruptured aneurysms, or erosion by malignancies. The rapid blood loss associated with major vessel bleeding can lead to hypovolemic shock, organ ischemia, and, if not swiftly managed, death. Effective management requires immediate control of bleeding, often through direct pressure, vessel clamping, or the application of hemostatic agents, followed by definitive surgical repair and aggressive volume resuscitation. Air Embolism: Air embolism occurs when air enters the vascular system and forms bubbles that obstruct blood flow. Venous air embolism (VAE) is more common due to the lower pressures in the venous system but can be equally dangerous. Arterial air embolism (AAE), though less common, can occur during certain surgical procedures or when air passes through cardiac septal defects. These air bubbles can travel to vital organs, causing ischemia and potentially severe complications such as stroke, myocardial infarction, or pulmonary embolism. Immediate management involves positioning the patient to trap air in less critical areas, administering 100% oxygen, and in severe cases, utilizing hyperbaric oxygen therapy. Risk Factors: - Surgical Procedures: Cardiovascular surgeries, thoracic surgeries, and neurosurgeries are particularly high-risk due to the involvement of major blood vessels and the potential for air introduction. - Trauma: Penetrating injuries and severe blunt trauma can damage major vessels. - Medical Conditions: Conditions such as cancer, severe infections, and connective tissue disorders can weaken vessel walls, increasing the risk of rupture. Clinical Manifestations: - Major Vessel Bleeding: Signs include hemodynamic instability, visible external bleeding, internal hematoma formation, and organ dysfunction. - Air Embolism: Symptoms range from sudden dyspnea, chest pain, and hypotension (in VAE) to neurological deficits and acute ischemia (in AAE). Diagnosis: Early and accurate diagnosis is crucial. Techniques include ultrasonography, computed tomography (CT) scans, transesophageal echocardiography (TEE), and intraoperative monitoring tools such as capnography and precordial Doppler ultrasound. Management Strategies: - For Major Vessel Bleeding: Immediate bleeding control, surgical repair, and postoperative intensive care. - For Air Embolism: Preventive measures during surgery, immediate patient positioning, air aspiration, and hyperbaric oxygen therapy. Conclusion: The successful management of major vessel bleeding and air embolism hinges on prompt recognition, effective intraoperative techniques, and comprehensive postoperative care. Continuous advancements in surgical technology and techniques, along with ongoing education and research, are vital to further reducing the incidence and impact of these life-threatening complications in surgical practice.
Similar Videos