Dr. Steven D. Wexner’s Insights from WALS 2025 Consensus Statement
Add to
Share
114 views
Report
1 month ago
Description
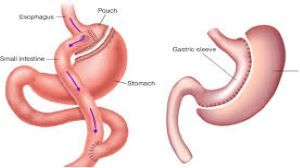
Fluorescence-Guided Surgery: Dr. Steven D. Wexner’s Insights from WALS 2025 Consensus Statement Fluorescence-guided surgery (FGS) represents a transformative advancement in modern surgical practice, leveraging near-infrared light and fluorescent dyes like indocyanine green (ICG) to enhance intraoperative visualization and decision-making. At the forefront of this evolving field is Dr. Steven D. Wexner, a globally recognized colorectal surgeon and Director of the Ellen Leifer Shulman and Steven Shulman Digestive Disease Center at Cleveland Clinic Florida. His contributions to the development and application of FGS, particularly in colorectal surgery, have been pivotal. During the 8th World Congress of Laparoscopic Surgeons (WALS) 2025, held on February 27, 2025, at The Leela Ambience Gurugram, Dr. Wexner shared critical insights as part of a consensus statement on fluorescence-guided surgery, reflecting years of research, clinical expertise, and collaborative efforts with international experts. This article delves into Dr. Wexner’s perspectives, the WALS 2025 Consensus Statement, and the broader implications of FGS in surgical innovation. Background on Fluorescence-Guided Surgery FGS is a technique that uses fluorescent agents, typically ICG, which emit light in the near-infrared spectrum when excited by specific wavelengths. This fluorescence is captured by specialized imaging systems, enabling surgeons to visualize structures and physiological processes that are invisible under traditional white light. Over the past decade, FGS has gained traction across surgical disciplines, including colorectal, oncologic, and reconstructive surgery, for applications such as assessing tissue perfusion, identifying lymphatic drainage, localizing tumors, and protecting critical anatomical structures. In colorectal surgery, one of the most promising applications of FGS is the reduction of anastomotic leaks—a devastating complication with leak rates as high as 20% in low colorectal anastomoses. By providing real-time visualization of blood flow, FGS allows surgeons to optimize anastomosis placement, potentially improving patient outcomes. Dr. Wexner has been a pioneer in exploring these applications, contributing to a growing body of evidence that underscores the safety and efficacy of FGS. Dr. Steven D. Wexner: A Leader in Surgical Innovation Dr. Wexner’s credentials are extensive and distinguished. As Chairman of the Department of Colorectal Surgery at Cleveland Clinic Florida since 1993, he has trained thousands of surgeons worldwide and published over 1,000 manuscripts and 270 textbook chapters. His leadership extends to roles such as past president of the American Society of Colon and Rectal Surgeons and vice-chair of the Board of Regents of the American College of Surgeons. His work in FGS builds on a legacy of innovation, including the development of the double-stapled ileo-anal pouch and the Wexner incontinence score. At WALS 2025, Dr. Wexner’s participation was a highlight, given his deep involvement in prior consensus efforts, such as the 2019 Delphi survey of international FGS experts and his authorship of key publications like "Indocyanine Green Fluorescence Guided Surgery in Colorectal Surgery" (Journal of Clinical Medicine, 2023). His insights at WALS 2025 bridged clinical practice with emerging research, offering a roadmap for the future of FGS. The WALS 2025 Consensus Statement: Key Takeaways The WALS 2025 Consensus Statement, presented during the congress, was the culmination of discussions among leading laparoscopic surgeons, including Dr. Wexner, aimed at standardizing and advancing the use of FGS. While the full text of the statement is not yet publicly available as of February 28, 2025, Dr. Wexner’s remarks during a dedicated session (aired on YouTube on February 27, 2025) provide a window into its core themes. Below are the key takeaways, informed by his presentation and aligned with his prior work: 1. Efficacy and Safety of FGS - Dr. Wexner emphasized that FGS, particularly with ICG, is widely regarded as both effective and safe across diverse surgical settings. At WALS 2025, he reiterated findings from earlier studies, such as the 2019 Delphi survey, where 19 international experts reached consensus on 41 of 44 statements affirming FGS’s utility in localizing critical structures (e.g., ureters, blood vessels), assessing perfusion, and mapping lymphatics. He noted that the technique’s safety profile is bolstered by ICG’s long history of use and minimal adverse effects. 2. Applications in Colorectal Surgery - A cornerstone of Dr. Wexner’s contribution was his focus on colorectal surgery, where FGS has shown particular promise. He highlighted its role in reducing anastomotic leaks by allowing surgeons to assess bowel perfusion intraoperatively. At WALS, he cited evidence suggesting that perfusion assessment should prioritize the anastomotic site over tumor location—a principle he first articulated in a 2017 interview with Annals of Translational Medicine. He also showcased case examples from his practice, such as ureter identification during pelvic dissection and sentinel lymph node mapping, reinforcing FGS’s versatility. 3. Need for Standardization - Despite its benefits, Dr. Wexner stressed the variability in FGS application, echoing concerns from prior consensus efforts. At WALS 2025, he advocated for standardized protocols regarding patient preparation, dye administration (e.g., timing and dosage of ICG), and imaging technology. He argued that such guidelines are essential to optimize outcomes and facilitate broader adoption, particularly in laparoscopic and robotic platforms. 4. Future Directions and Research Gaps - Looking ahead, Dr. Wexner underscored the need for rigorous clinical trials to quantify FGS’s impact on patient outcomes, such as leak rates and cancer recurrence. He also pointed to emerging innovations, like tumor-targeted fluorescent probes and artificial intelligence integration for real-time microcirculation analysis, as areas ripe for exploration. At WALS, he encouraged collaboration between surgeons, researchers, and industry to address these gaps. 5. Education and Training - A recurring theme in Dr. Wexner’s address was the importance of training. He noted that while FGS is intuitive, its effective use requires familiarity with imaging systems and interpretation of fluorescence signals. He proposed integrating FGS into surgical residency programs and leveraging platforms like WALS to disseminate best practices globally. Conclusion Dr. Steven D. Wexner’s insights from the WALS 2025 Consensus Statement underscore the transformative potential of fluorescence-guided surgery while highlighting the work still needed to fully realize its benefits. His leadership in colorectal surgery, combined with his collaborative efforts at WALS, positions FGS as a cornerstone of modern operative care. As of February 28, 2025, the surgical community stands at a pivotal moment—armed with a consensus framework and a call to action from one of its most respected voices. Whether through reducing complications, enhancing oncologic precision, or training the next generation, Dr. Wexner’s vision for FGS promises a future where surgeons see better to do better, ultimately improving lives one procedure at a time.
Similar Videos