Single vs. Multiple Laparoscopic Surgeries: Comparative Insights from WALS 2025
Add to
Share
146 views
Report
1 month ago
Description
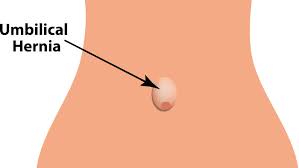
Single vs. Multiple Laparoscopic Surgeries: Comparative Insights from WALS 2025 Laparoscopic surgery, often referred to as minimally invasive surgery, has revolutionized modern surgical practices by offering patients reduced recovery times, smaller incisions, and lower risks of complications compared to traditional open surgery. As the field continues to evolve, debates surrounding the efficacy, safety, and applicability of single-incision laparoscopic surgery (SILS) versus multiple-incision laparoscopic surgery (MILS) have gained prominence. The World Association of Laparoscopic Surgeons (WALS) 2025 Congress, held on February 8-9 in Gurugram, India, provided a critical platform for surgeons, researchers, and medical professionals to present cutting-edge insights into this ongoing comparison. This article delves into the comparative insights from WALS 2025, exploring the advantages, challenges, and future directions of single versus multiple laparoscopic surgeries. Understanding Single and Multiple Laparoscopic Surgeries Laparoscopic surgery utilizes small incisions through which a laparoscope—a thin tube equipped with a camera and light—is inserted, allowing surgeons to visualize and operate on internal organs. In traditional multiple-incision laparoscopic surgery (MILS), several small ports (typically 3-5) are created to accommodate the laparoscope and various instruments. This approach has been widely adopted across specialties, including general surgery, gynecology, and urology, for procedures such as cholecystectomy (gallbladder removal), appendectomy, and hysterectomy. Single-incision laparoscopic surgery (SILS), also known as single-port laparoscopy, takes minimal invasiveness a step further by consolidating all instruments and the laparoscope into a single entry point, often at the umbilicus. Introduced in the late 1990s and gaining traction in the 2000s, SILS aims to reduce scarring, improve cosmetic outcomes, and potentially decrease postoperative pain. However, its technical complexity and limited applicability have sparked ongoing discussions about its place in surgical practice compared to the more established MILS. At WALS 2025, experts from around the globe presented data-driven analyses, live surgical demonstrations, and case studies to compare these two approaches, shedding light on their clinical outcomes, technical feasibility, and patient satisfaction. Clinical Outcomes: A Head-to-Head Comparison One of the central themes at WALS 2025 was the evaluation of clinical outcomes between SILS and MILS. Studies presented at the congress highlighted both similarities and differences across key metrics such as operative time, postoperative pain, complication rates, and recovery duration. Operative Time Multiple studies underscored that SILS often requires longer operative times than MILS, particularly for complex procedures. The single-port approach limits instrument triangulation—a cornerstone of laparoscopic surgery—making it more challenging to maneuver tools effectively. For instance, a retrospective analysis of laparoscopic cholecystectomies showed that SILS procedures averaged 15-20 minutes longer than their MILS counterparts. This difference was attributed to the learning curve and the need for specialized instruments. However, surgeons with extensive SILS experience reported narrowing this gap, suggesting that proficiency plays a significant role. Postoperative Pain and Recovery A key promise of SILS is reduced postoperative pain due to fewer incisions. WALS 2025 data offered mixed insights. Some studies, including a prospective cohort study on appendectomies, reported statistically significant reductions in pain scores at 24 and 48 hours post-surgery for SILS patients. Others, however, found no notable difference, particularly when MILS incisions were small (e.g., 5 mm ports). Recovery times generally aligned with pain outcomes: SILS patients often resumed normal activities slightly faster, though hospital stays were comparable between the two groups in most cases.
Similar Videos