Sphincter Salvage Surgery for Rectal Cancer: Key Takeaways from WALS 2025
Add to
Share
112 views
Report
1 month ago
Description
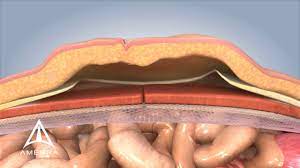
Sphincter salvage surgery represents a pivotal advancement in the treatment of low rectal cancer, aiming to preserve the anal sphincter and thereby maintain continence, avoiding the need for a permanent colostomy. The World Association of Laparoscopic Surgeons (WALS) 2025 conference shed light on the latest developments and key considerations in this domain, emphasizing patient selection, surgical techniques, functional outcomes, and multidisciplinary approaches. Patient Selection Criteria The success of sphincter-preserving procedures heavily relies on meticulous patient selection. Ideal candidates typically present with tumors located in the lower third of the rectum, specifically within 5 cm of the anal verge, without invasion into the external sphincter or levator ani muscles. Preoperative assessments, including high-resolution magnetic resonance imaging (MRI) and endorectal ultrasonography, are crucial for evaluating tumor extent and its relationship to surrounding structures. Additionally, factors such as tumor size, stage, and response to neoadjuvant therapy play significant roles in determining eligibility for sphincter-preserving surgery. citeturn0search1 Advancements in Surgical Techniques Several innovative surgical techniques have emerged to enhance the feasibility and outcomes of sphincter-preserving surgeries: - Intersphincteric Resection (ISR): This technique involves the partial or total removal of the internal anal sphincter to achieve clear distal margins while preserving the external sphincter. Studies have demonstrated that ISR can be performed safely with low local recurrence rates and satisfactory functional outcomes, making it a viable alternative to abdominoperineal resection (APR) for selected patients. citeturn0search2 - Transanal Endoscopic Microsurgery (TEM) and TransAnal Minimally Invasive Surgery (TAMIS): These minimally invasive approaches allow for precise local excision of early-stage rectal tumors. TEM and TAMIS are associated with reduced postoperative pain, shorter hospital stays, and quicker recovery times compared to traditional open surgeries. citeturn0search1 - Transanal Total Mesorectal Excision (TaTME): TaTME combines transanal and laparoscopic abdominal approaches to facilitate meticulous dissection of the mesorectum, particularly in patients with mid to low rectal cancers. This technique offers improved visualization and may result in better oncological outcomes. citeturn0search1 Functional Outcomes and Quality of Life While sphincter-preserving surgeries aim to maintain continence, they can be associated with postoperative functional challenges collectively known as low anterior resection syndrome (LARS). Symptoms of LARS include increased stool frequency, urgency, incontinence, and a sensation of incomplete evacuation. These issues can significantly impact a patient's quality of life. Management strategies encompass dietary modifications, pelvic floor rehabilitation, medications, and, in some cases, surgical interventions. Comprehensive preoperative counseling and postoperative support are essential to address these potential functional impairments. citeturn0search6 Multidisciplinary Approach and Accreditation Standards The WALS 2025 conference underscored the importance of a multidisciplinary approach in the management of rectal cancer. Collaboration among colorectal surgeons, medical and radiation oncologists, radiologists, pathologists, and specialized nursing staff is vital for optimizing treatment outcomes. The American College of Surgeons' National Accreditation Program for Rectal Cancer (NAPRC) has introduced updated standards to ensure comprehensive and coordinated care. These standards emphasize the significance of multidisciplinary team meetings, standardized treatment protocols, and continuous quality improvement initiatives. citeturn0search7 Conclusion Sphincter salvage surgery for rectal cancer has evolved considerably, offering patients the possibility of maintaining continence without compromising oncological safety. The insights from WALS 2025 highlight the critical aspects of patient selection, advancements in surgical techniques, management of functional outcomes, and the necessity of a multidisciplinary approach. As research and clinical practices advance, these strategies are poised to further enhance patient outcomes and quality of life in rectal cancer care.
Similar Videos