Safe Laparoscopic Hysterectomy with ICG Fluorescence Imaging
Add to
Share
16 views
Report
3 days ago
Description
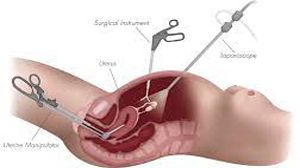
Safe Laparoscopic Hysterectomy with ICG Fluorescence Imaging Laparoscopic hysterectomy, a minimally invasive surgical procedure to remove the uterus, has become a preferred approach due to its benefits, including reduced recovery time, minimal scarring, and lower complication rates compared to open surgery. The integration of Indocyanine Green (ICG) fluorescence imaging into this procedure has further enhanced its safety and precision, offering surgeons real-time visualization of critical anatomical structures. This advanced technology is transforming gynecologic surgery by improving outcomes and reducing risks. What is ICG Fluorescence Imaging? Indocyanine Green (ICG) is a non-toxic, fluorescent dye that, when injected intravenously, binds to plasma proteins and fluoresces under near-infrared light. When used with specialized imaging systems, ICG allows surgeons to visualize blood vessels, bile ducts, and tissue perfusion in real-time during surgery. In the context of laparoscopic hysterectomy, ICG fluorescence imaging provides a clear map of vascular structures and tissue viability, enabling precise surgical navigation. Benefits of ICG in Laparoscopic Hysterectomy 1. Enhanced Visualization of Anatomy During a hysterectomy, identifying key structures like the ureters, uterine arteries, and surrounding vasculature is critical to avoid complications such as bleeding or organ injury. ICG fluorescence highlights these structures with high clarity, reducing the risk of inadvertent damage. For example, ureteral visualization with ICG helps surgeons avoid ureteral injuries, which, though rare, can lead to significant complications. 2. Improved Blood Supply Assessment ICG enables real-time assessment of tissue perfusion, ensuring that surrounding organs, such as the ovaries or bladder, maintain adequate blood flow after the uterus is removed. This is particularly valuable in complex cases, such as those involving endometriosis or large fibroids, where distorted anatomy may obscure normal vascular patterns. 3. Reduced Operative Complications By providing a detailed view of the surgical field, ICG fluorescence minimizes the likelihood of intraoperative complications, such as excessive bleeding or unintended injury to adjacent organs. Studies have shown that ICG-guided surgery can lower the incidence of postoperative complications, including infections and hematomas. 4. Support for Complex Cases In patients with prior surgeries, pelvic adhesions, or abnormal anatomy, ICG fluorescence offers a significant advantage. It allows surgeons to navigate challenging conditions with greater confidence, ensuring safer outcomes even in high-risk scenarios. 5. Minimally Invasive Precision Laparoscopic hysterectomy already offers precision through small incisions and high-definition cameras. Adding ICG fluorescence complements this by providing an additional layer of intraoperative guidance, aligning with the minimally invasive ethos of reduced trauma and faster recovery. Procedure Overview During a safe laparoscopic hysterectomy with ICG fluorescence imaging: 1. Preoperative Preparation: The patient is evaluated to determine the suitability of a laparoscopic approach. ICG is prepared for administration, and the surgical team ensures the availability of a near-infrared imaging system. 2. ICG Administration: The dye is injected intravenously at specific points during the procedure, depending on the structures being visualized (e.g., ureters or blood vessels). 3. Real-Time Imaging: The laparoscopic camera, equipped with near-infrared capabilities, captures the fluorescence emitted by ICG. Surgeons monitor the illuminated structures on a screen, guiding their dissection and ligation. 4. Uterus Removal: The uterus is carefully detached from its supporting ligaments and blood vessels, with ICG ensuring precise identification of critical anatomy. 5. Closure and Recovery: After confirming tissue perfusion and hemostasis, the procedure is completed, and the patient is monitored for a smooth recovery. Safety Considerations While laparoscopic hysterectomy with ICG is generally safe, certain precautions are essential: - Allergic Reactions: ICG is well-tolerated, but rare allergic reactions may occur. Patients with a history of iodine or contrast allergies are screened beforehand. - Surgeon Expertise: The procedure requires specialized training in both laparoscopy and fluorescence-guided surgery to maximize benefits. - Equipment Availability: Access to near-infrared imaging systems is necessary, which may not be available in all surgical centers. Clinical Evidence and Outcomes Research supports the safety and efficacy of ICG fluorescence in laparoscopic hysterectomy. Studies indicate a reduction in intraoperative complications, shorter operative times, and improved patient outcomes when ICG is used. For instance, a 2023 meta-analysis found that ICG-guided hysterectomy reduced ureteral injury rates by up to 50% compared to standard laparoscopy. Additionally, patients benefit from shorter hospital stays and faster return to daily activities. Future Directions The adoption of ICG fluorescence imaging is expanding as technology advances. Innovations such as robotic-assisted laparoscopy with integrated ICG systems and artificial intelligence-guided imaging are poised to further enhance surgical precision. As more surgeons are trained in fluorescence-guided techniques, the approach is likely to become a standard of care in gynecologic surgery. Conclusion Safe laparoscopic hysterectomy with ICG fluorescence imaging represents a significant advancement in gynecologic surgery. By providing real-time visualization of critical structures, ICG enhances surgical precision, reduces complications, and improves patient outcomes. For women requiring hysterectomy, this approach offers a minimally invasive, highly effective option that prioritizes safety and recovery. As technology continues to evolve, ICG-guided surgery will undoubtedly play a pivotal role in shaping the future of gynecologic care.
Similar Videos